About ACMS
The American College of Mohs Surgery (ACMS) is a membership organization of fellowship-trained skin cancer and reconstructive surgeons specializing in the Mohs micrographic surgical technique used to treat skin cancer.
The ACMS serves as the voice of the specialty, promoting and advancing the highest standards of patient care through fellowship training, research, education and public advocacy.
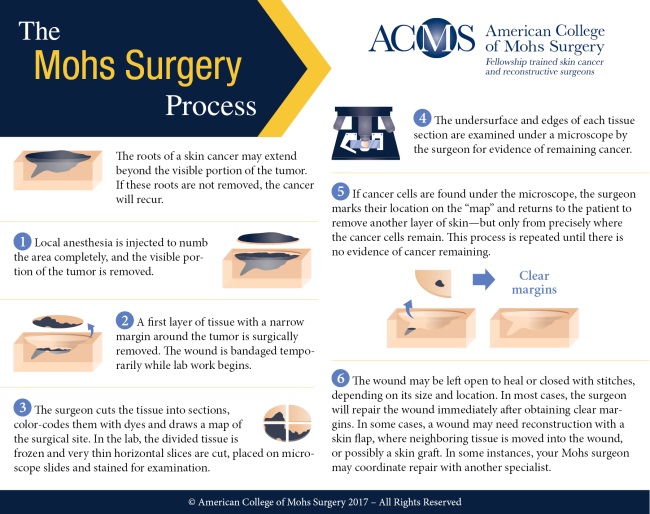
The organization was founded in 1967 by Dr. Frederic E. Mohs and a small group of surgeons who had begun to use Dr. Mohs' technique. Mohs pioneered a highly specialized and precise technique that removes skin cancer in stages, one tissue layer at a time, resulting in minimal damage to the surrounding healthy tissue and the highest potential cure rate, at up to 99%. Dr. Mohs served as the first president of the College.
The procedure has advanced considerably over the years and the College has grown to nearly 1,500 members, all of whom have received advanced fellowship training in Mohs surgery, pathology, and reconstructive surgery. The ACMS is the only organization that requires its members to have successfully completed an extensive one- to two-year fellowship training program in Mohs surgery after they have completed their years of dermatology residency training. During their fellowships, physicians participate in at least 500 Mohs surgery cases under the supervision of an experienced Mohs surgeon.
To learn whether Mohs surgery is an appropriate treatment for your skin cancer, find a fellowship trained Mohs surgeon in your area.
Learn More
- About Mohs Surgery
- History of Mohs Surgery and the ACMS
- Why Choose a Fellowship Trained Mohs Surgeon?
- Mohs Micrographic Surgery Overview
- Why Does My Cancer Need Mohs Surgery?
- The Mohs Procedure
- Post-Operative Care